
How Inflammation and Diet Are Connected: A Science-Based Guide to Eating for Recovery
How Inflammation and Diet Are Connected: A Science-Based Guide to Eating for Recovery
Your body's inflammatory response doesn't operate in isolation from what you eat. Every meal you consume either fans the flames of chronic inflammation or helps dampen them through complex biochemical pathways that researchers have spent decades mapping. Understanding this connection gives you practical leverage over conditions ranging from joint pain to metabolic syndrome.
What Happens in Your Body When Diet Triggers Inflammation
When you eat foods that promote inflammation, your immune system responds as if facing a threat. Certain dietary components trigger the release of pro-inflammatory cytokines—signaling proteins like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) that coordinate immune responses. While these molecules serve protective functions during acute injuries or infections, their chronic elevation creates tissue damage.
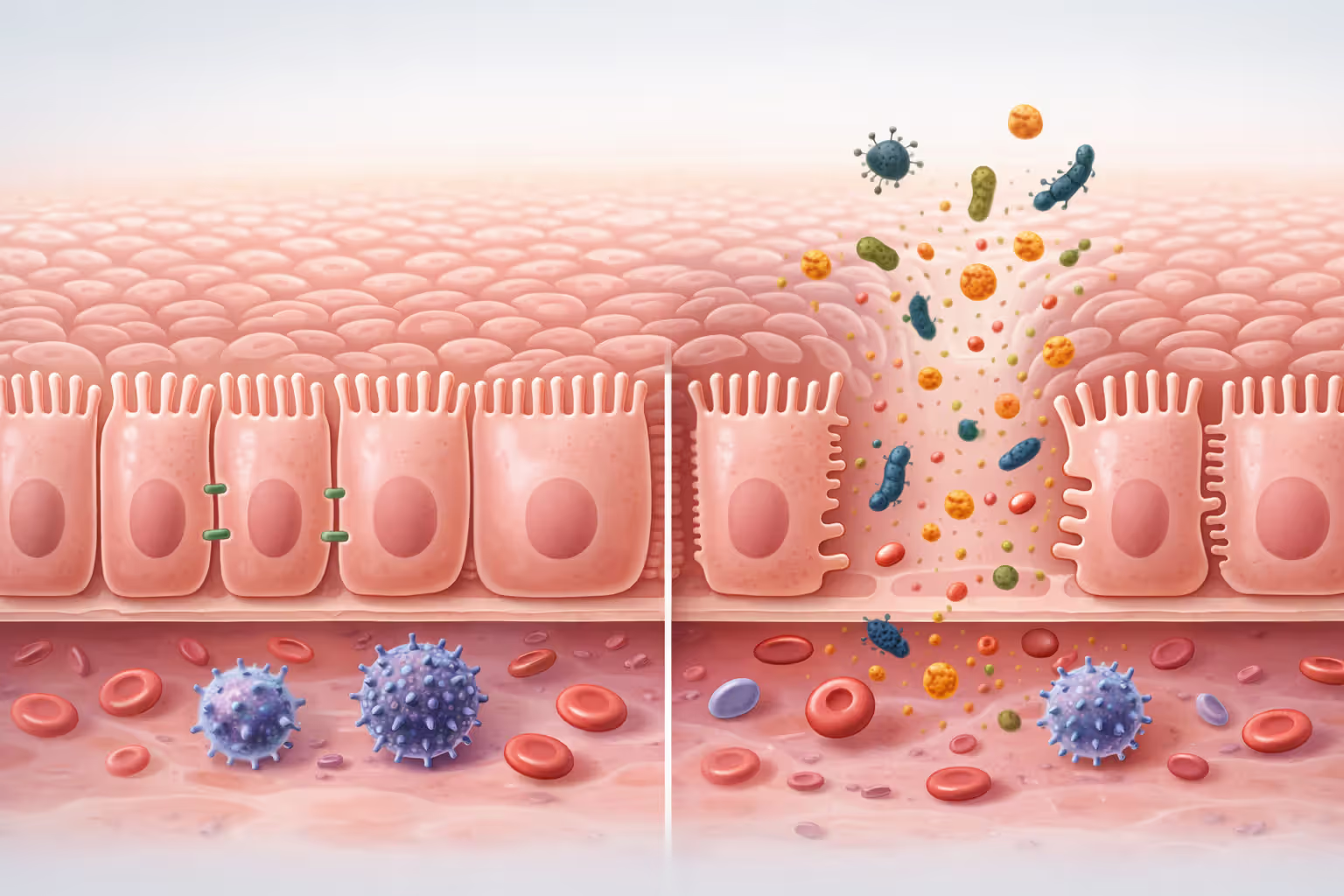
The process begins in your gut. Foods high in refined sugars and damaged fats increase intestinal permeability, sometimes called "leaky gut." This allows bacterial fragments called lipopolysaccharides (LPS) to cross into your bloodstream. Your immune system recognizes these molecules as foreign invaders and mounts a defensive response, releasing inflammatory mediators that circulate throughout your body.
Oxidative stress amplifies this cascade. When you consume foods that generate excessive free radicals—unstable molecules that damage cells—your body's antioxidant defenses can become overwhelmed. This imbalance triggers nuclear factor kappa B (NF-κB), a protein complex that acts like a master switch for inflammatory gene expression. Once activated, NF-κB tells your cells to produce more inflammatory molecules, creating a self-reinforcing cycle.
Advanced glycation end products (AGEs) represent another mechanism linking inflammation and diet. These compounds form when proteins or fats combine with sugars at high temperatures. They accumulate in tissues and bind to cell surface receptors called RAGEs, which then activate inflammatory pathways. Your body can handle small amounts of dietary AGEs, but chronic exposure from heavily processed and charred foods overwhelms clearance mechanisms.
Author: Jessica Taylor;
Source: thelifelongadventures.com
The relationship between chronic inflammation food science and metabolic health centers on adipose tissue. When you consistently overeat inflammatory foods, fat cells enlarge and begin secreting their own inflammatory cytokines. These adipokines alter insulin signaling and contribute to systemic inflammation that affects organs far from the original fat deposits.
Foods That Raise Inflammation Markers: What the Research Shows
Eat food. Not too much. Mostly plants.
— Michael Pollan
Refined Carbohydrates and Added Sugars
White bread, pastries, and sugar-sweetened beverages spike blood glucose rapidly, triggering insulin surges that promote inflammatory signaling. A 2018 study in the American Journal of Clinical Nutrition found that participants consuming high-glycemic diets showed 29% higher C-reactive protein (CRP) levels compared to those eating low-glycemic alternatives.
The fructose component of added sugars poses particular problems. Unlike glucose, which every cell can metabolize, fructose processing occurs primarily in the liver. Excessive intake overwhelms hepatic pathways, leading to fat accumulation, oxidative stress, and increased production of uric acid—all of which elevate inflammation markers. Regular soda consumption has been linked to elevated IL-6 and TNF-α in multiple cohort studies.

Author: Jessica Taylor;
Source: thelifelongadventures.com
Trans Fats and Oxidized Oils
Partially hydrogenated oils and repeatedly heated cooking fats contain trans fatty acids and oxidized lipids that directly damage cell membranes. These altered fats integrate into cellular structures, making them more susceptible to inflammatory damage. Research published in the Journal of Nutrition demonstrated that trans fat intake correlates with elevated CRP, IL-6, and soluble adhesion molecules—markers of vascular inflammation.
Vegetable oils high in omega-6 fatty acids aren't inherently inflammatory, but the typical American diet contains a ratio of omega-6 to omega-3 fatty acids around 15:1, when ancestral diets maintained ratios closer to 4:1. This imbalance shifts eicosanoid production toward pro-inflammatory compounds like prostaglandin E2 and leukotriene B4.
Processed Meats and High-AGE Foods
Bacon, hot dogs, and deli meats contain preservatives like sodium nitrite that can form N-nitroso compounds—potent inflammatory agents. Beyond additives, the high-heat processing creates abundant AGEs. A single serving of bacon contains roughly 11,000 AGE units, while the same amount of raw meat contains fewer than 1,000 units.
Grilled and fried foods accumulate AGEs exponentially. Chicken breast cooked at 350°F for 15 minutes contains about 1,000 AGE units, but the same chicken grilled at 450°F for the same duration contains over 5,000 units. These compounds persist in your body for weeks, continuously activating RAGE receptors and sustaining inflammatory responses.
| Food Category | Primary Inflammatory Compounds | Associated Markers | Evidence Strength |
| Refined carbohydrates & added sugars | Glucose spikes, fructose metabolites | CRP, IL-6, TNF-α | Strong |
| Trans fats & oxidized oils | Trans fatty acids, lipid peroxides | CRP, IL-6, adhesion molecules | Strong |
| Processed meats | AGEs, N-nitroso compounds, heme iron | CRP, IL-6, TNF-α | Strong |
| High-heat cooked foods | AGEs, heterocyclic amines | RAGE activation, oxidative markers | Moderate |
| Alcohol (excess) | Acetaldehyde, endotoxins | CRP, IL-6, liver enzymes | Strong |
| Artificial additives | Emulsifiers, certain preservatives | Gut barrier markers, systemic CRP | Emerging |
Anti-Inflammatory Nutrients Your Body Actually Needs
Omega-3 fatty acids—specifically EPA and DHA from marine sources—compete with omega-6 fatty acids for the same metabolic enzymes. This competition shifts eicosanoid production away from inflammatory prostaglandins toward resolvins and protectins, specialized molecules that actively resolve inflammation rather than simply suppressing it. Clinical trials show that 2-4 grams daily of combined EPA/DHA can reduce CRP by 15-30% within eight weeks.
Polyphenols from colorful plants inhibit NF-κB activation and reduce oxidative stress through multiple pathways. Curcumin from turmeric blocks inflammatory enzyme COX-2 with potency comparable to some pharmaceutical anti-inflammatories. Quercetin from onions and apples stabilizes mast cells, preventing excessive histamine release. Resveratrol activates sirtuins—proteins that regulate cellular stress responses and reduce inflammatory gene expression.

Author: Jessica Taylor;
Source: thelifelongadventures.com
Fiber serves anti-inflammatory functions beyond simple digestive health. Soluble fiber from oats, beans, and vegetables feeds beneficial gut bacteria that produce short-chain fatty acids (SCFAs) like butyrate. These SCFAs strengthen intestinal barriers, reducing LPS leakage, and directly signal immune cells to adopt anti-inflammatory profiles. Studies show that each 10-gram daily increase in fiber intake correlates with roughly 10% lower CRP levels.
Vitamin D functions more like a hormone than a vitamin, with receptors on immune cells throughout your body. Adequate vitamin D status—generally above 30 ng/mL serum 25-hydroxyvitamin D—helps regulate T-cell responses and reduces production of inflammatory cytokines. Observational studies consistently link vitamin D deficiency with elevated inflammation markers, though supplementation trials show mixed results depending on baseline status.
Magnesium acts as a natural calcium channel blocker and NF-κB inhibitor. This mineral is required for over 300 enzymatic reactions, including those that neutralize free radicals. Population studies reveal that people consuming adequate magnesium (320-420 mg daily) show 25-40% lower CRP levels than those with insufficient intake. Dark leafy greens, nuts, seeds, and whole grains provide bioavailable magnesium that processed diets lack.
| Nutrient | Best Food Sources | Daily Target | Primary Mechanism | Markers Reduced |
| Omega-3 (EPA/DHA) | Salmon, sardines, mackerel | 2-4g combined | Resolvin production, enzyme competition | CRP, IL-6, TNF-α |
| Polyphenols | Berries, green tea, dark chocolate, turmeric | 500-1000mg | NF-κB inhibition, antioxidant activity | CRP, oxidative stress markers |
| Soluble fiber | Oats, beans, Brussels sprouts, apples | 10-15g | SCFA production, gut barrier support | CRP, IL-6, endotoxin levels |
| Vitamin D | Fatty fish, fortified foods, sunlight | 1000-2000 IU (to maintain 30+ ng/mL) | Immune cell regulation | CRP, IL-6 (if deficient) |
| Magnesium | Spinach, almonds, black beans, avocado | 320-420mg | NF-κB inhibition, antioxidant enzyme cofactor | CRP, IL-6 |
| Vitamin E | Sunflower seeds, almonds, hazelnuts | 15mg (22 IU) | Lipid peroxidation prevention | Oxidized LDL, IL-6 |
Building a Recovery Nutrition Plan to Lower Chronic Inflammation
Meal Timing and Inflammation Cycles
Your inflammatory status fluctuates throughout the day, influenced by circadian rhythms and feeding patterns. Cortisol—which has anti-inflammatory properties—peaks in early morning, making this period ideal for foods that might otherwise trigger stronger responses. Conversely, inflammatory markers naturally rise in the evening, suggesting that late-night eating of pro-inflammatory foods compounds existing elevation.
Eating within a consistent 10-12 hour window supports circadian alignment of metabolic processes. When you eat erratically or late into the night, you disrupt the normal rhythm of inflammatory gene expression. Research on time-restricted eating shows that confining meals to daylight hours reduces oxidative stress markers even when total calorie intake remains constant.
Post-exercise nutrition presents a special case. Intense training temporarily elevates inflammatory markers as part of normal adaptation, but this acute inflammation differs from chronic systemic inflammation. Consuming anti inflammatory nutrients within two hours after training—particularly omega-3s, polyphenols, and quality protein—supports recovery without suppressing beneficial adaptation signals.
Portion Strategies That Support Immune Balance
Overeating at individual meals triggers inflammatory responses regardless of food quality. Large portions spike blood glucose and triglycerides, activating NF-κB and generating oxidative stress. Studies using continuous glucose monitors reveal that keeping post-meal glucose below 140 mg/dL minimizes inflammatory spikes.
Author: Jessica Taylor;
Source: thelifelongadventures.com
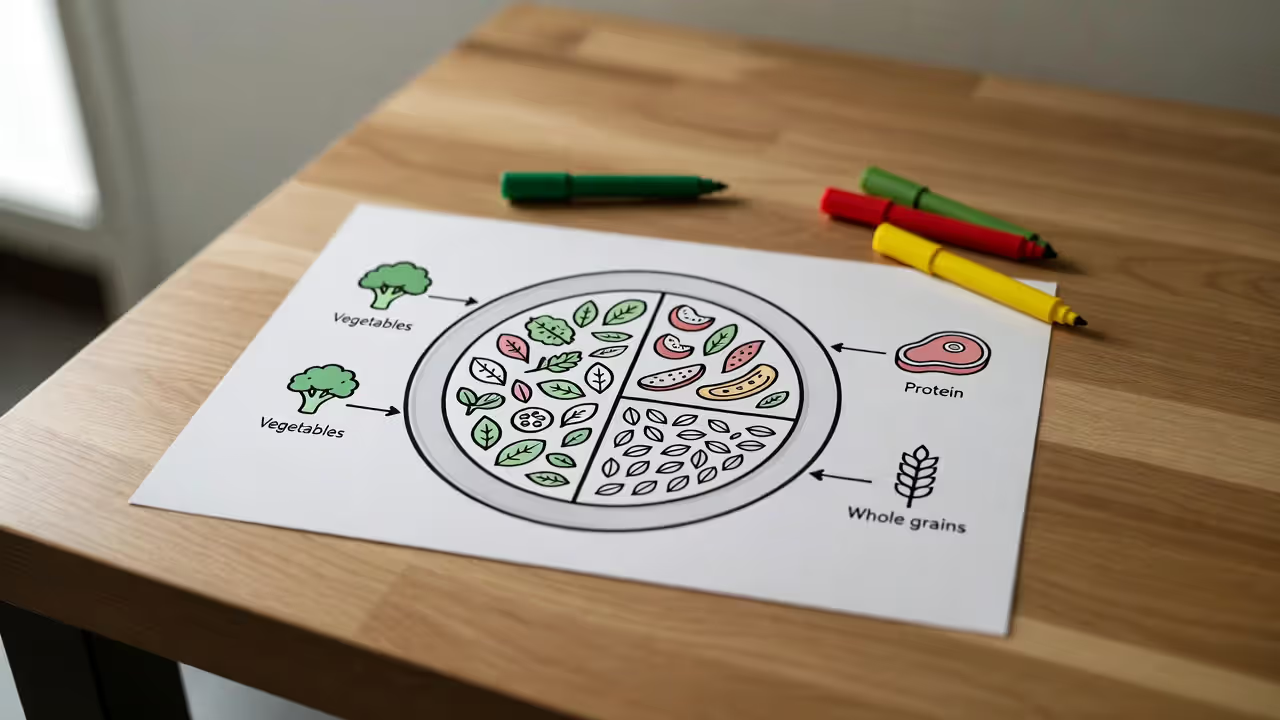
A practical framework: fill half your plate with non-starchy vegetables, one quarter with protein sources low in AGEs (poached fish, slow-cooked chicken, legumes), and one quarter with intact whole grains or starchy vegetables. This ratio naturally provides fiber, polyphenols, and balanced macronutrients while limiting inflammatory triggers.
Including small amounts of anti-inflammatory fats at each meal—extra virgin olive oil, avocado, nuts, or seeds—improves absorption of fat-soluble polyphenols and vitamins while moderating glucose responses. The Mediterranean dietary pattern, which emphasizes these principles, consistently reduces inflammation markers by 20-40% in intervention studies.
Recovery nutrition inflammation strategies should account for individual variability. Some people show strong inflammatory responses to specific foods due to genetic variations in immune receptors or gut microbiome composition. Tracking your response to dietary changes through symptoms and, when possible, inflammation markers helps personalize your approach beyond general guidelines.
How Long Does It Take Diet Changes to Affect Inflammation Levels?
Acute inflammatory markers respond surprisingly quickly to dietary shifts. Studies measuring CRP after switching from a Western diet to a Mediterranean-style diet show detectable reductions within two weeks, with more substantial changes—typically 25-35% decreases—appearing by six to eight weeks. IL-6 and TNF-α follow similar timelines.
has-data-writing-block:pointer-events-none has-data-writing-block:-mt-(--shadow-height) has-data-writing-block:pt-(--shadow-height) )>*]:pointer-events-auto scroll-mt-" tabindex="-1" dir="auto" data-turn-id="request-WEB:88a63ab1-f063-482e-b2f0-055bb94f07bf-1" data-testid="conversation-turn-4" data-scroll-anchor="true" data-turn="assistant"> @w-sm/main: @w-lg/main: px-(--thread-content-margin)"> @w-lg/main: mx-auto max-w-(--thread-content-max-width) flex-1 group/turn-messages focus-visible:outline-hidden relative flex w-full min-w-0 flex-col agent-turn" tabindex="-1">:mt-1" data-message-author-role="assistant" data-message-id="4a7022ca-65df-418d-a553-43fb659b6cfe" dir="auto" data-message-model-slug="gpt-5-2-thinking">">Let food be thy medicine and medicine be thy food.
— Hippocrates
Gut-mediated changes occur even faster. Intestinal permeability begins improving within days of removing highly processed foods and adding fermented foods and fiber. Beneficial bacteria populations shift within a week, though establishing a stable, healthy microbiome requires several months of consistent dietary patterns.
Tissue-level changes take longer. AGE deposits in collagen and other long-lived proteins require months to years to turn over. If you've consumed a high-AGE diet for decades, accumulated tissue damage won't reverse in weeks. However, stopping new AGE accumulation immediately reduces ongoing inflammatory stimulation.
Metabolic adaptations follow a middle timeline. Insulin sensitivity improvements—which reduce inflammatory signaling—become measurable within four to six weeks of consistent dietary changes. Adipose tissue remodeling, where inflamed fat cells shrink and reduce cytokine secretion, requires three to six months of sustained caloric balance or deficit.
Weight loss, when needed, accelerates inflammation reduction but isn't strictly necessary. Normal-weight individuals with elevated inflammation markers still benefit substantially from anti-inflammatory dietary patterns. However, each 10% reduction in excess body weight typically correlates with 20-30% decreases in CRP and other markers.
Realistic expectations matter. If your CRP started at 8 mg/L (high risk), dietary changes might bring it to 3-4 mg/L (moderate risk) within three months—significant improvement, but not complete normalization. Achieving levels below 1 mg/L often requires addressing multiple lifestyle factors beyond diet alone: sleep quality, stress management, physical activity, and environmental exposures.
Common Mistakes That Keep Inflammation High Despite "Healthy" Eating
Many people replace soda with fruit juice, not realizing that 12 ounces of orange juice contains similar sugar content (about 30 grams) and triggers comparable glucose and insulin spikes. Without the fiber present in whole fruit, juice provides concentrated fructose that promotes hepatic inflammation. Even "cold-pressed" and "no sugar added" varieties cause these effects.
Granola and trail mix marketed as health foods often contain more added sugars and oxidized oils than their conventional counterparts. A typical serving of commercial granola delivers 12-15 grams of added sugars plus rancid polyunsaturated fats from nuts stored improperly or processed at high heat. Making your own from fresh ingredients and storing it properly avoids these pitfalls.
"Natural" sweeteners like agave nectar contain 70-90% fructose—higher than high-fructose corn syrup at 55%. Honey and maple syrup, while containing beneficial compounds, still spike blood sugar when used liberally. Dates and date paste provide fiber alongside sugars, making them preferable options, but portion control remains essential.
Nuts and seeds provide anti inflammatory nutrients, but excessive consumption backfires. A handful (about 1 ounce) offers beneficial fats and polyphenols, but three or four handfuls add significant omega-6 fatty acids and calories that can promote inflammation when they displace other nutrient-dense foods. Rancid nuts—common when buying in bulk or storing improperly—contain oxidized fats that directly trigger inflammatory pathways.
Some foods labeled as "superfoods" cause problems for susceptible individuals. Nightshade vegetables (tomatoes, peppers, eggplants) contain alkaloids that trigger inflammation in people with specific sensitivities, though they're beneficial for most people. Similarly, lectins in improperly prepared beans and grains can increase intestinal permeability in some individuals, while others tolerate them well.
Supplement overreliance creates a false sense of security. Taking curcumin or fish oil capsules doesn't compensate for a diet built on processed foods. Whole-food sources provide synergistic compounds—fiber, vitamins, minerals, and hundreds of phytonutrients—that work together in ways isolated supplements cannot replicate. Supplements fill specific gaps but cannot replace dietary foundation.
Aggressive elimination diets sometimes increase stress and social isolation, which elevate cortisol and inflammatory markers independent of food choices. Unless you have confirmed allergies or intolerances, overly restrictive eating may cause more harm than benefit. A balanced anti-inflammatory diet includes wide variety within beneficial food categories.
Frequently Asked Questions About Diet and Inflammation
Moving Forward With Inflammation-Conscious Eating
The relationship between inflammation and diet operates through well-established biological mechanisms that you can influence daily through food choices. Unlike genetic factors you cannot change, dietary patterns remain largely within your control, offering practical leverage over inflammatory status that affects everything from joint pain to metabolic health.
Start by identifying and reducing your primary inflammatory triggers rather than attempting perfect eating overnight. If you currently drink soda daily, replacing it with water or unsweetened tea will likely reduce your inflammation markers more than adding a turmeric supplement while keeping the soda. If you eat fast food regularly, cooking simple meals at home from whole ingredients creates bigger changes than debating whether to buy organic.
Build your diet around foods that actively reduce inflammation: fatty fish twice weekly, colorful vegetables at most meals, berries and nuts as snacks, extra virgin olive oil as your primary fat, beans and lentils several times weekly, and herbs and spices liberally. This positive framework proves more sustainable than restrictive elimination approaches for most people.
Monitor your response through both subjective measures—energy levels, joint comfort, digestive function, skin quality—and objective markers when accessible. Improvements in how you feel often precede measurable changes in blood markers, but both matter. If you're not seeing progress after three months of consistent dietary changes, consider working with a healthcare provider to identify other contributing factors or individual food sensitivities.
Remember that reducing chronic inflammation through diet represents a long-term commitment rather than a quick fix. The inflammatory damage from years of poor eating won't reverse in weeks, but every anti-inflammatory meal moves you toward better health. Small, consistent improvements compound over time into substantial changes in inflammation markers, symptom burden, and disease risk.
Related Stories

Read more

Read more

The content on this website is provided for general informational and educational purposes related to health, yoga, fitness, and overall wellness. It is not intended to replace professional medical advice, diagnosis, or treatment.
All information, workout suggestions, yoga practices, nutrition tips, and wellness guidance shared on this site are for general reference only. Individual health conditions, fitness levels, and medical needs vary, and results may differ from person to person. Always consult a qualified healthcare provider before starting any new exercise program, dietary plan, or wellness routine.
We are not responsible for any errors or omissions, or for any outcomes resulting from the use of information presented on this website. Your health and fitness decisions should always be made in consultation with appropriate medical and fitness professionals.




